What is Endometriosis; a guide to symptoms, causes and treatment options
Endometriosis is a chronic and often painful condition that affects approximately 1 in 9 women, but unfortunately a lot of women still battle the symptoms of endometriosis in silence. In this article, we shed light on its causes, symptoms, diagnostic methods, available treatments, and the impact on the lives of those who experience it.
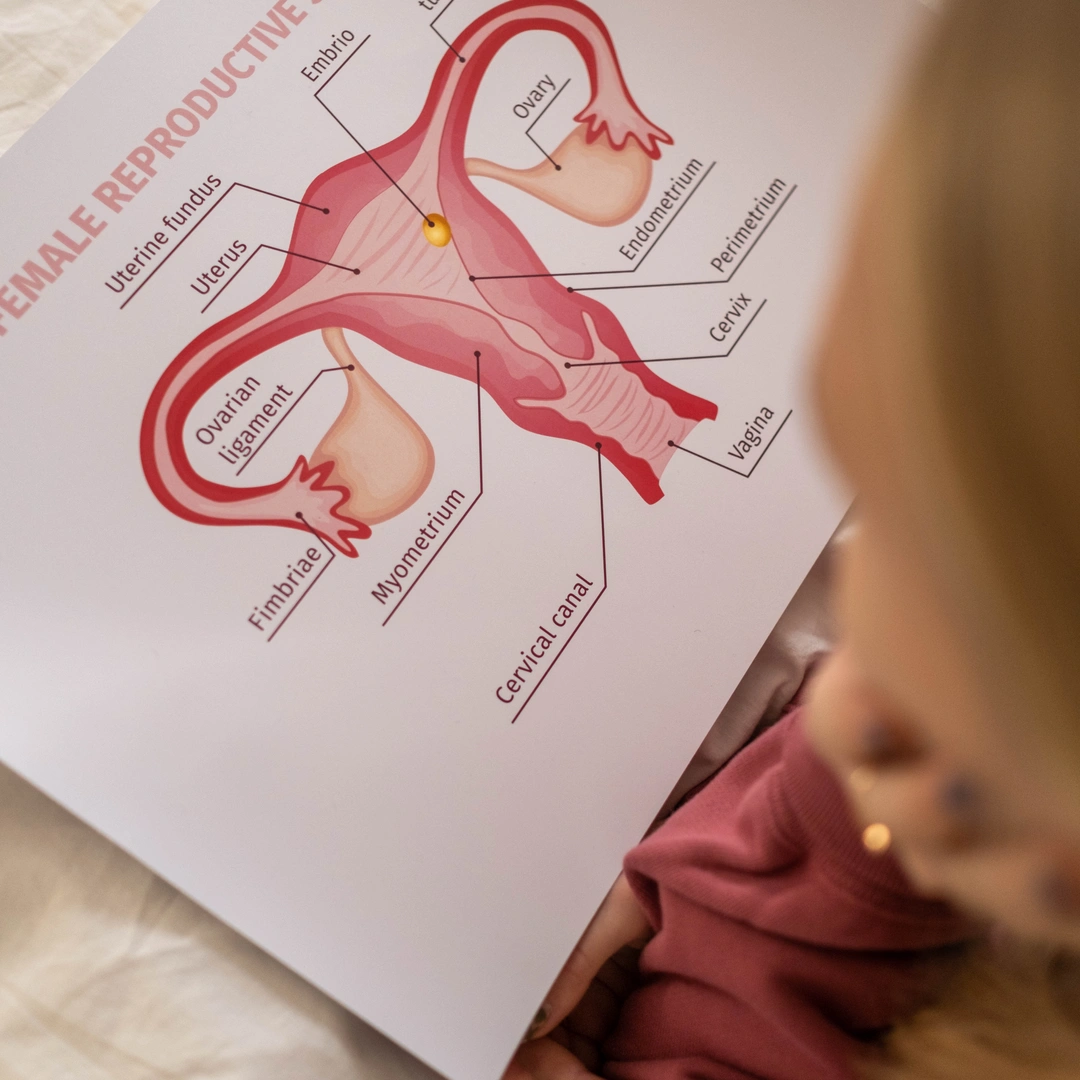 Image credit:
Cotton Bro Studio
Image credit:
Cotton Bro Studio
Introduction
Endometriosis is a chronic and often painful condition that affects millions of women worldwide. Although endometriosis affects approximately 1 in 9 women of reproductive age globally, it remains a topic that needs to be more widely discussed and is often misunderstood. Often, women battle the symptoms of endometriosis in silence. It can be challenging to find the right treatment, and unfortunately, there's currently no definite cure. You can, however, regain control over your health and well-being and manage your symptoms with the correct information and support.
What is Endometriosis?
Endometriosis is a medical condition in which tissue similar to the lining of the uterus, called the endometrium, grows outside the uterus. It primarily affects the reproductive organs, such as the ovaries, fallopian tubes, and the tissues lining the pelvis. This abnormal growth can lead to painful lesions, adhesions, and cysts.
Prevalence
Endometriosis is estimated to affect approximately 1 in 10 women of reproductive age globally and 1 in 9 women in Australia. It is most commonly diagnosed in women between 25 and 40 but can also affect teenagers and women approaching menopause. Despite its prevalence, endometriosis is often misdiagnosed or undiagnosed, causing delayed treatment and unnecessary suffering for women.
Symptoms
The symptoms of endometriosis can vary from mild to severe, and they may not always correlate with the extent of the disease. Common symptoms include:
Pelvic Pain
Heavy or Irregular periods
Chronic Fatigue
Painful urination or bowel movements
Infertility
-
Pelvic pain: Women with endometriosis often experience pelvic pain ranging from mild discomfort to debilitating cramps, especially during menstruation or sexual intercourse.
-
Heavy or irregular periods: Menstrual flow that is excessively heavy or irregular can indicate endometriosis.
-
Chronic fatigue: Many women with endometriosis report feeling exhausted despite ample rest and sleep.
-
Painful urination or bowel movements: Endometrial tissue growth can cause pain during urination or bowel movements, especially during menstruation.
-
Infertility: Endometriosis can also impact fertility, making it difficult for women to conceive.

What causes Endometriosis?
The exact cause of endometriosis is unknown, and more research is needed. Below, we will discuss potential contributors.
-
Genetic and Hormonal Influences: Research suggests that genetic and hormonal factors play a significant role in the development of endometriosis. If your close relatives, such as your mother, sister, or aunt, have been diagnosed with this condition, your risk of developing it may be higher. Hormonal imbalances, such as estrogen dominance, may also contribute to the growth of endometrial tissue outside the uterus.
-
Role of Immune System Dysfunction: The immune system is crucial to maintaining the body's health. In the case of endometriosis, immune system dysfunction may be a contributing factor. When the immune system fails to recognise and eliminate endometrial tissue growing outside the uterus, it allows the condition to progress. This dysfunction may be due to genetic factors, environmental triggers, or other underlying health conditions.
-
Environmental and Lifestyle Factors: While genetics and hormones are significant factors, environmental and lifestyle choices can also impact the risk of developing endometriosis. Some studies suggest that exposure to certain environmental toxins, such as dioxins and PCBs found in pesticides, plastics, and industrial chemicals, may increase the likelihood of developing endometriosis. Lifestyle factors such as excessive alcohol consumption and a sedentary lifestyle may also contribute to the risk.
-
Inflammatory and Autoimmune Conditions: Certain inflammatory and autoimmune conditions, such as allergies, asthma, and autoimmune diseases, have been associated with an increased risk of endometriosis. These conditions may create a pro-inflammatory environment in the body, promoting the growth and spread of endometrial tissue outside the uterus.
How is Endometriosis diagnosed?
Several tests can help diagnose endometriosis:
-
Pelvic exam: Your doctor can manually examine your pelvis for cysts, scar tissues and other abnormalities. It's important to note that small areas of endometriosis may not always be detectable during this exam.
-
Ultrasound: This test utilises high-frequency sound waves to create images of the inside of your body. The transducer, a device used in the test, is either inserted into your vagina (transvaginal ultrasound) or placed on your abdomen to obtain the best view of your reproductive organs. While a standard ultrasound cannot definitively diagnose endometriosis, it can help identify cysts associated with the condition known as endometriomas.
-
Magnetic resonance imaging (MRI): An MRI is a thorough examination that employs a magnetic field and radio waves to generate detailed images of your organs and tissues. In some instances, an MRI can benefit surgical planning, providing your surgeon with precise information about the location and size of endometrial implants.
-
Laparoscopy: Sometimes, your doctor may refer you to a surgeon for a laparoscopy. This procedure allows the surgeon to inspect your abdomen and determine if you have endometriosis.
What are the treatment options?
While endometriosis has no cure, several treatment options can help manage the symptoms and improve quality of life. Treatment plans are usually tailored to the individual and may include:
-
Pain medication: Over-the-counter anti-inflammatory pain relievers such as ibuprofen can help alleviate mild to moderate pain associated with endometriosis.
-
Hormonal therapy: Birth control pills, hormonal patches, or intrauterine devices can help regulate hormonal imbalances and menstrual cycles and reduce symptoms. In some cases, gonadotropin-releasing hormone (GnRH) agonists or antagonists may be recommended by a doctor to suppress the production of estrogen, which can help slow the growth of endometrial tissue.
-
Surgery: In severe cases, laparoscopic surgery may be recommended to remove endometrial tissue, scar tissue, cysts, or adhesions. This approach aims to alleviate pain and improve fertility. Laparoscopy is a minimally invasive procedure, often requiring an overnight stay at the hospital. During laparoscopy, a small incision is made near your belly button, and a slender viewing instrument called a laparoscope is inserted to search for signs of endometrial tissue outside the uterus. This procedure can provide valuable information about the endometrial implants' location, extent, and size. Additionally, your surgeon may take a tissue sample (biopsy) for further testing. In some cases, your surgeon may be able to fully treat endometriosis during the laparoscopy, eliminating the need for multiple surgeries. In more severe cases, a hysterectomy may be considered, which involves the removal of the uterus. However, this option is typically reserved for women who no longer wish to have children or for whom other treatments have been ineffective.
-
Complementary Therapies: Many women with endometriosis seek alternative and complementary therapies to supplement conventional treatments. These therapies can aid in pain management, reduce stress, and improve overall well-being. Acupuncture, yoga, mindfulness meditation, and dietary modifications are popular options. While these approaches may not directly treat endometriosis, they can provide relief from associated symptoms and enhance overall quality of life.
-
Lifestyle Modifications: Lifestyle changes: Adopting a healthy lifestyle, incorporating regular exercise, managing stress levels, and maintaining a balanced diet can help reduce symptoms. Reducing or avoiding inflammatory foods, such as processed foods and excessive caffeine, may also alleviate symptoms for some women. Maintaining a healthy weight and managing stress levels can also help manage endometriosis.
Having extreme pain during your periods is not something you need to accept.
Endometriosis is a complex, chronic condition that affects millions of women worldwide. Increasing awareness and understanding can provide better support and care for those living with endometriosis. While there is no definitive cure, several effective treatment options are available for symptom management and improving your overall quality of life. Each woman's experience with endometriosis is unique, and treatment plans should be personalised in consultation with healthcare professionals. By combining medication therapy, alternative therapies, lifestyle modifications and, in some instances, surgical interventions, women can take control of their health and relieve the challenges posed by endometriosis. If you think you might have endometriosis, please don't hesitate to contact your doctor to discuss. Having extreme pain during your periods is not something you have to accept and there are treatment options available.
Share this article
Cannabis & endometriosis. How Cannabis can help reduce inflammation and symptoms
Endometriosis affects 1 in 9 Australian girls, women and those who are assigned female at birth. The pain caused by endometriosis can be so severe that people who experience it may not be able to participate in their daily activities. Cannabis could not only help relieve endometriosis symptoms, but new research shows that medicinal marijuana could potentially reduce lesions associated with endometriosis.

